I. Follicular Phase:
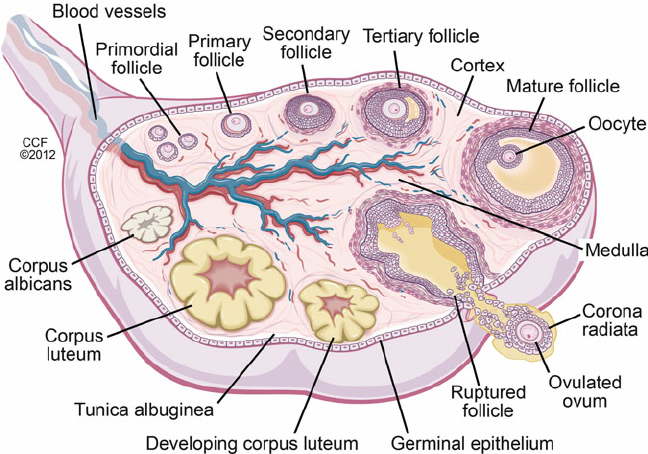
The follicular phase is the initial stage of the menstrual cycle, marked by the development and maturation of ovarian follicles. It begins on the first day of menstruation and lasts until ovulation. During this phase, the hypothalamus releases gonadotropin-releasing hormone (GnRH), which stimulates the anterior pituitary gland to release follicle-stimulating hormone (FSH). FSH, in turn, acts on the ovaries, promoting the growth and development of several follicles. As the follicles mature, they produce estrogen, which has various effects on the body. Estrogen stimulates the thickening of the uterine lining (endometrium) in preparation for potential implantation and inhibits further FSH production to prevent excessive follicle development. Eventually, one dominant follicle emerges and continues to mature, while the others undergo atresia. The follicular phase concludes with a surge in luteinizing hormone (LH), triggered by rising estrogen levels, which sets the stage for ovulation and the subsequent luteal phase of the menstrual cycle.
A. Follicle-Stimulating Hormone (FSH)
- Initiates follicular development in the ovaries
- Stimulates the production of estrogen
B. Estrogen
- Promotes the proliferation of the endometrium
- Inhibits follicle-stimulating hormone (FSH) to prevent excessive follicle development
- Stimulates the production of luteinizing hormone (LH)
C. Luteinizing Hormone (LH)
- Surge in LH triggers ovulation
- Induces the development of the corpus luteum
Read how to lose weight without exercise
II. Ovulation:
Ovulation in humans refers to the release of a mature egg (oocyte) from the ovary into the fallopian tube. It is a crucial event in the menstrual cycle and typically occurs around the midpoint of the cycle, approximately 14 days before the start of the next menstrual period. Ovulation is triggered by a surge in luteinizing hormone (LH) levels, which is primarily stimulated by high levels of estrogen. This surge causes the dominant ovarian follicle, which has been developing during the follicular phase, to rupture and release the mature egg.
The egg is then swept into the fallopian tube, where it awaits fertilization by sperm. Ovulation is a brief process, usually lasting only a few minutes to hours. It marks the fertile period of a woman’s menstrual cycle, and successful fertilization during this time can lead to pregnancy. If fertilization does not occur, the unfertilized egg disintegrates, and the woman enters the subsequent luteal phase, leading to menstruation and the beginning of a new cycle.
A. Luteinizing Hormone (LH)
- Surge in LH levels causes the dominant follicle to rupture and release the mature egg
- Initiates the conversion of the ruptured follicle into the corpus luteum
III. Luteal Phase:
The luteal phase is a stage of the menstrual cycle that follows ovulation and precedes menstruation. It is characterized by the presence and activity of the corpus luteum, which forms from the ruptured ovarian follicle after the release of the egg during ovulation. The luteal phase typically lasts for about 10 to 16 days and is marked by significant hormonal changes.
Once the egg is released, the ruptured follicle undergoes a transformation and becomes the corpus luteum. The corpus luteum primarily produces progesterone, along with smaller amounts of estrogen and other hormones. Progesterone plays a crucial role in preparing the uterus for possible embryo implantation.
During the luteal phase, the increased levels of progesterone and estrogen contribute to the thickening of the uterine lining (endometrium), making it more receptive to a fertilized egg. The endometrium develops a rich blood supply and glandular secretions to support embryo implantation.
If fertilization occurs during the luteal phase, the fertilized egg implants itself into the thickened endometrium, leading to pregnancy. The corpus luteum continues to produce progesterone, maintaining the endometrium and supporting the early stages of pregnancy until the placenta takes over hormone production.
However, if fertilization does not occur, the corpus luteum gradually regresses, leading to a decrease in progesterone and estrogen production. As hormone levels decline, the endometrium is no longer sustained, and it begins to break down. This breakdown results in the shedding of the endometrial lining, leading to menstrual bleeding and the start of a new menstrual cycle.
The length of the luteal phase remains relatively constant for each individual, typically ranging from 10 to 16 days. Monitoring the length of the luteal phase is important in assessing the overall health of a woman’s menstrual cycle and fertility. A consistently short luteal phase, known as luteal phase defect, may pose challenges for successful implantation and can be associated with fertility issues.
A. Corpus Luteum
- Secretes progesterone
- Supports the maintenance of the endometrium for potential embryo implantation
- Inhibits the production of FSH and LH to prevent further ovulation
B. Progesterone
- Thickens the endometrium, preparing it for potential implantation
- Suppresses the immune response to protect a developing embryo
- Prepares the mammary glands for potential lactation
IV. Menstruation:
Menstruation, also known as a menstrual period or simply a period, is a natural process that occurs in humans with reproductive capacity. It is a crucial part of the menstrual cycle and refers to the monthly shedding of the uterine lining (endometrium) when pregnancy does not occur. Menstruation typically lasts for about 3 to 7 days, but the duration can vary from person to person. The onset of menstruation, known as menarche, usually begins during puberty and continues until menopause.
During menstruation, hormonal changes, specifically a decrease in progesterone and estrogen levels, trigger the release of substances that cause the blood vessels in the endometrium to constrict and the lining to break down. This results in the menstrual flow, which consists of blood, mucus, and tissue from the uterus, exiting the body through the vagina. Menstruation serves as an indicator of reproductive health and plays a significant role in the reproductive cycle, preparing the uterus for potential pregnancy in the subsequent menstrual cycle
A. Decreased Levels of Estrogen and Progesterone
- Withdrawal of hormonal support leads to endometrial shedding
- Initiates menstrual bleeding
Conclusion: Summary of roles of hormones in menstrual cycle
The menstrual cycle is a highly regulated process involving a precise sequence of hormonal events. Understanding the roles of hormones in each phase is essential for medical students. From follicular development to ovulation, corpus luteum formation, and menstrual shedding, hormones play a critical role at every step. By grasping this intricate dance, medical students can develop a comprehensive understanding of reproductive physiology and provide better care to their patients in the future.