Table of Contents
Introduction
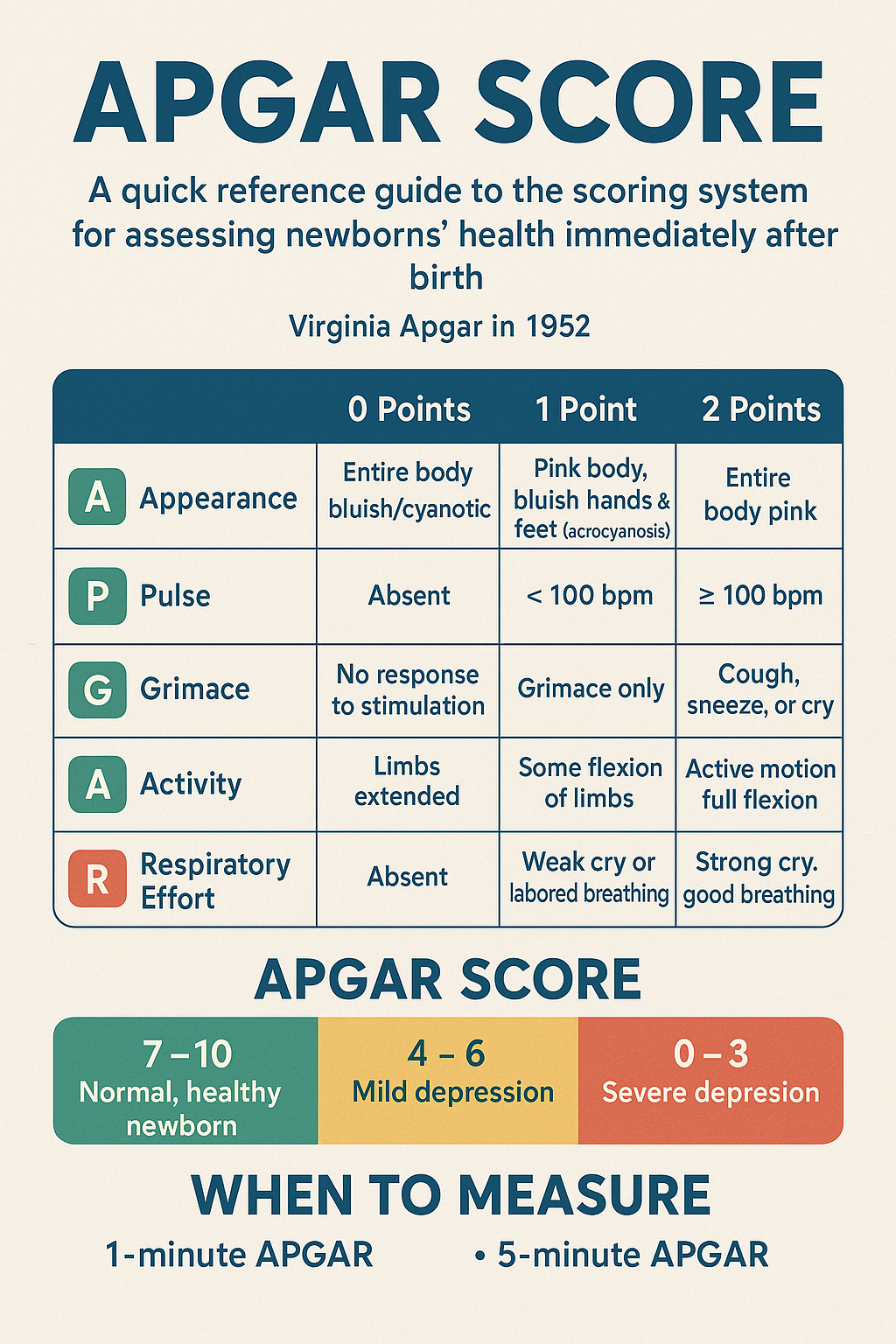
The APGAR score is a rapid method to assess the health status of a newborn immediately after birth.
It was introduced in 1952 by Dr. Virginia Apgar, an American anesthesiologist, to provide an objective and standardized evaluation.
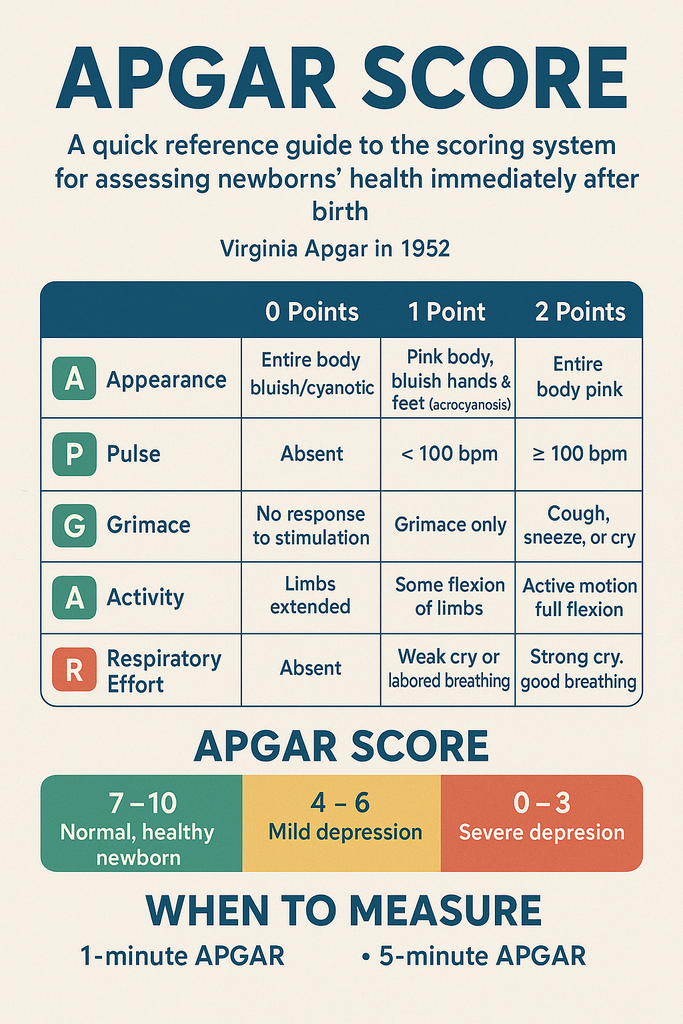
The score is based on five parameters, each evaluated at 1 minute and 5 minutes after birth, with each parameter scored from 0 to 2. The maximum score is 10.
APGAR Parameters
| Letter | Parameter | 0 Points | 1 Point | 2 Points |
|---|---|---|---|---|
| A | Appearance (Skin Color) | Entire body bluish/cyanotic | Pink body, bluish hands & feet (acrocyanosis) | Entire body pink |
| P | Pulse (Heart Rate) | Absent | < 100 bpm | ≥ 100 bpm |
| G | Grimace (Reflex Response) | No response to stimulation | Grimace only | Cough, sneeze, or cry |
| A | Activity (Muscle Tone) | Limbs extended (flaccid) | Some flexion of limbs | Active motion, full flexion |
| R | Respiratory Effort | Absent | Weak cry or labored breathing | Strong cry, good breathing |
Interpreting the APGAR Score
- 7–10: Normal, healthy newborn
- 4–6: Mild depression (needs observation and possibly mild intervention)
- 0–3: Severe depression (needs urgent medical attention)
When to Measure
- 1-minute APGAR: Reflects the newborn’s condition at birth and initial adaptation to the environment.
- 5-minute APGAR: Evaluates the effectiveness of ongoing care and resuscitation efforts.
- If the 5-minute score is < 7, assessment should be repeated every 5 minutes up to 20 minutes.
Practical Note for Delivery Rooms
- Look & Listen: Appearance, activity, respiratory effort
- Feel: Heart rate, reflex response (grimace)
This quick check can be done within seconds and helps guide immediate care for the newborn.
Summary:
The APGAR score remains one of the simplest and most effective tools for assessing newborn well-being. It does not predict long-term outcomes but is essential for guiding immediate care and determining if urgent intervention is required.